Tuesday, December 22, 2009
Israel revamps its priority system for deceased donor organs
New Law For Organ Donation In Israel: Increased Priority For Those Who Are Prepared To Donate
"An article published Online First and in The Lancet reports that a unique new law comes into effect in Israel in January 2010. It states that people who are prepared to sign donor cards themselves receive priority when they are in need of an organ transplant. In addition, increased priority is given to first degree relatives of those who have signed donor cards, to first degree relatives of those who have died and given organs, and to live donors of a kidney, liver lobe or lung lobe who have donated for as yet undesignated recipients. The article is the work of Professor Jacob Lavee, Director of the Heart Transplantation Unit, Sheba Medical Centre, Ramat Gan, and the Israel Transplant Centre, and colleagues. "
...
"There are different levels of priority concerning the different situations. A transplant candidate with a first-degree relative who has signed a donor card would be given half the allocation priority that is given to a transplant candidate who has signed his or her own donor card. Then again, a transplant candidate with a first-degree relative who donated organs after death or who was an eligible live non-directed organ donor would be given allocation priority 1.5 times greater than that given to candidates who have signed their own donor cards. Among candidates with the same number of allocation points, organs will be allocated first to prioritisation-eligible candidates. Regardless of the new law, patients in urgent need of a heart, lung, or liver transplant due to their serious condition will continue to receive priority. However, in the event that two such people are eligible for the same organ, their priority status under the new law would decide who receives the organ. Candidates under 18 and those unable to express their wishes due to physical or mental disability will retain their priority status versus an adult who merits priority."
This priority system is more nuanced than the one enshrined in Singapore law (see the bottom of this post). And of course legislation on a national scale gives donors a priority for all deceased donor organs, not just those from like-minded donors, which is the path being taken by Lifesharers, an interesting organization about which I posted here.
HT: Steve Leider
Update: here's a YNet followup from March 2010 Radical way to boost organ donation.It discusses, among other things, political obstacles to implementing the new law...
Tuesday, March 19, 2024
The Impact of prioritization on kidney and liver allocation in Israel
Israel's Organ Transplantation Law grants some priority on waiting lists for transplants to candidates who are first-degree relatives of deceased organ donors (i.e. whose family has given permission for someone's deceased organ donation) or who previously registered as organ donors themselves. (There's also a tiny priority for relatives of people who signed organ donor cards...) Here are two papers that looks at the effect of those priorities on kidney and liver transplants, and how they interact with other priorities on waiting lists for Israeli organs.
The first paper, on kidneys, concludes that the priorities are effective in reducing waiting time to transplant, and suggests that perhaps these priorities should not be so large compared to other existing priorities (e.g. for time on dialysis), or for priorities that could be established, e.g. for highly sensitized patients (who get high priority in the U.S., for example.)
Mor, Eytan, Meitar Bloom, Ronen Ghinea, Roi Anteby, Ronit Pasvolsky-Gutman, Ron Loewenthal, Ido Nachmani, and Tammy Hod. "The Impact of the Donor Card Holder Prioritization Program on Kidney Allocation in Israel." Transplantation (2024): 10-1097.
Abstract
Background: Since 2014, as part of a priority program within the Israeli Transplant Law, additional points were given to waitlisted candidates with donor cards. We assessed the impact on deceased donor kidney allocation.
Methods: This study enrolled all patients older than 18 y who underwent deceased donor kidney transplantation (January 2016–December 2019). Data were obtained from the National HLA Tissue Laboratory registry at the Sheba Medical Center. Patients were grouped by donor card status (ADI group) (not signed, 0 points; relative signed, 0.1 points; patient signed, 2 points; and relative donated, 9 points). The primary outcome was waiting time until kidney transplantation with and without the additional score.
Results: Four hundred forty-four patients underwent kidney transplantation during the study period: 281 (63%) were donor card holders (DCH) and 163 (37%) were not DCH. DCH with extra points waited 68.0 (±47.0) mo on average, compared with 94.6 (±47.3) mo for not DCH (P < 0.001). Donor card signers had a shorter time until transplant in a multivariable model. Without extra points, 145 recipients (32.6%) would have missed organs allocated to higher-scored candidates. Allocation changes occurred in 1 patient because of an additional 0.1 points, in 103 candidates because of an additional 2 points, and in 41 candidates because of an additional 9 points.
Conclusions: Additional DCH scores improved allocation and reduced waiting time for donor card signers and those with donating relatives. To enhance fairness, consideration should be given to reducing the score weight of this social criterion and raising scores for other factors, especially dialysis duration.
##########
There are many fewer liver transplants than kidney transplants, and the effect of priority is less clear:
Ashkenazi, Tamar, Avraham Stoler, and Eytan Mor. "The effect of priority given to donor card holders on the allocation of livers for transplant—evidence from 7 years of the Israeli priority program." Transplantation 106, no. 2 (2022): 299-307.
Abstract
Background. The Israeli Transplant Law grants priority in organ allocation to patients signing a donor card. Liver transplant candidates get additional 2 points on their Model for End Stage Liver Disease score for signing a donor card, 0.1 points for a relative holding a card, and 5 points if a relative donated an organ. We studied the effect of the priority program on waiting list mortality and allocation changes due to priority.
Methods. Using Israeli Transplant data of 531 adult liver transplant candidates with chronic liver disease listed between 2012 and 2018 we compared waitlist mortality and transplant rate of candidates with and without priority. Then we analyzed liver allocations resulting from additional priority points and followed outcome of patients who were skipped in line.
Results. Of the 519 candidates, 294 did not sign a donor card, 82 signed, 140 had a relative sign, and for 3, a relative donated an organ. The rates of waitlist mortality in these 4 groups were 22.4%, 0%, 21.4%, and 0%, respectively, and the transplant rates were 50%, 59.8%, 49.3%, and 100%, respectively. Of the 30 patients who were skipped because of priority, 24 subsequently underwent transplant, 2 are on the waiting list, and 4 died within 0.75, 1.75, 7, and 17 mo.
Conclusions. The 2 points added to the Model for End Stage Liver Disease score were associated with lower waitlist mortality and higher transplant rate for candidates signing a donor card without significantly affecting access to transplant during allocation. Further research and consideration of optimal policy when granting priority for candidates signing a donor card should continue.
###########
Earlier:
Stoler, Avraham, Judd B. Kessler, Tamar Ashkenazi, Alvin E. Roth, Jacob Lavee, “Incentivizing Authorization for Deceased Organ Donation with Organ Allocation Priority: the First Five Years,” American Journal of Transplantation, Volume 16, Issue 9, September 2016, 2639–2645.
Stoler, Avraham, Judd B. Kessler, Tamar Ashkenazi, Alvin E. Roth, Jacob Lavee, “Incentivizing Organ Donor Registrations with Organ Allocation Priority,”, Health Economics, April 2016 Volume: 26 Issue: 4 Pages: 500-510 APR 2017
Saturday, August 24, 2013
Organ donation in Britain: will it follow Israel's lead?
Registered organ donors could be given priority for transplants
"Patients who have agreed to donate organs could be given priority if they ever need a transplant, under proposals being considered by the NHS.
...
"In a report published today (THURS) NHS Blood and Transplant published a new plan to improve organ donations.
"The report floats one approach where patients already on the Organ Donor Register would be given higher priority for transplants should they need one.
"Professor James Neuberger, associate medical director at NHS Blood and Transplant, said: “They do this in Israel and it has encouraged donation.
“It was first introduced in Singapore. While they don’t exclude those who don’t donate, it gives priority to those who are on the donor register.
“Whether it is appropriate for the UK is up for debate and discussion.”
"Any move to prioritise patients on the donor register would require a decision by ministers and a change in organ allocation rules."
******************
The subject will be debated at the upcoming National Donation and Transplantation Congress, which is being held at the University of Warwick in early September.
Here's the announcement of the debate, with Jay Lavee, the Israeli heart transplant surgeon who has been at the heart of the change to priority in Israel speaking in favor (and presumably some of the others speaking against...)
Here is the UK Organ Donation and Transplantation site, and here are some links to the NHS Blood and Transplant Service documents on current proposals:
Taking Organ Transplantation to 2020
 Here's the accompanying full report (pdf)
Here's the accompanying full report (pdf)The table is from that report, summarizing the goals and current situation.
Here are other earlier posts following Jay Lavee's work
Monday, January 23, 2023
Incentives for deceased organ donation, in Asia
Here's a discussion, in an Asian context, of providing incentives to families to consent to deceased donation.
Introducing Incentives and Reducing Disincentives in Enhancing Deceased Organ Donation and Transplantation by Kai Ming ChowMBChB⁎ Curie AhnMD† Ian DittmerMBChB‡ Derrick Kit-SingAuLMCHK§ IanCheungMBBS║ Yuk LunChengMBChB¶ Chak SingLau MBChB Deacons Tai-KongYeungMBBS║ Philip Kam-TaoLi MD Seminars in Nephrology, Available online 27 December 2022
*Department of Medicine and Therapeutics, Carol and Richard Yu PD Research Centre, Prince of Wales Hospital, The Chinese University of Hong Kong, Shatin, Hong Kong
† Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, South Korea
‡Department of Renal Medicine, Auckland City Hospital, Faculty of Medical and Health Sciences, University of Auckland, Auckland, New Zealand
§Centre for Bioethics, Faculty of Medicine, The Chinese University of Hong Kong, Shatin, Hong Kong
║Cluster Services Division, Hospital Authority, Kowloon, Hong Kong
¶Department of Medicine, Alice Ho Miu Ling Nethersole Hospital, Tai Po, Hong Kong
#Department of Medicine, Queen Mary Hospital, University of Hong Kong, Pok Fu Lam, Hong Kong, China
Summary: Despite the effectiveness of solid organ transplantation, progress to close the gap between donor organs and demand remains slow. An organ shortage increases the waiting time for transplant and involves significant costs including patient morbidity and mortality. Against the background of a low deceased organ donation rate, this article discusses the option of introducing incentives and removing disincentives to deceased organ donation. Perspectives from ethics, general public opinion, and the health care profession are examined to ensure a comprehensive appraisal and illustrate different facets of opinion on this complex area. Special cultural and psychosocial considerations in Asia, including the family based consent model, are discussed.
This sentence caught my eye:
"After suggestion by Economics Nobel Laureate Alvin Roth for the community to unite to remove disincentives to kidney donation, the transplant community and academia have been having more discussion and analysis. That, in part, hinges on the estimates of the economic welfare gain for the society as a whole."
...
"PERSPECTIVES OF ASIAN SOCIETY
"It is widely recognized that deceased organ donation rates in Asian countries have been significantly lower than that in Western countries.
...
"No one disputes the social and cultural beliefs in the decision to donate organs.
...
"An example of honoring the principles of reciprocity in incentivizing organ donor registrations is the organ allocation priority policy. Israel became the first country in 2008 to enact legislation incorporating such incentives based on individuals’ willingness to donate into their organ procurement system.26,42,43 The policy provides an incentive or motivation by the reciprocal altruistic dictum that “each partner helping the other while he helps himself,”42 granting priority on organ donor waiting lists to those individuals who registered as organ donors by signing a donor card for at least 3 years. Subsequent observations in Israel, as analyzed 5 years after introduction of the new policy, included an increase in the authorization rate of next of kin of unregistered donors, as well as a two-fold higher likelihood of next-of-kin authorization for donation when the deceased relative was a registered donor.44
"How does the concept of reciprocity apply for Asian societies? Will the results from Israel be replicated in Asia? Although social exchange theory should be a universal normal applicable to all human relationships, cultural influence or patterns might differ. Previous research on reciprocity across different cultural contexts, indeed, has shown that East Asians tend to reciprocate in kind and emphasize more on equity-based theory than Americans.45 Viewed through such a lens of “to give is to take,” it is relevant to quote another similar example in Taiwan, where incentives were provided to deceased organ donors’ families. In brief, after a person has become a deceased organ donor in Taiwan, up to three of his or her blood relatives will be granted priority to receive a deceased donor organ should they be on the waiting list for transplantation.46
"At the heart of the issue is the family based consent that is unique and vital, albeit not exclusive, in Confucian tradition within Chinese societies. It is important to note that organ donation is more often a family based consent process in Chinese culture than those “from a Western cultures”. As such, family priority right provided in the Israel or Chinese model would be more likely to motivate organ donation within a family based ethical culture.47 As in any discussion of culture's influence on organ donation decision, we must be mindful that East Asians tend to favor family centered decision making.
...
"If the concept of reimbursing funeral expenses for deceased organ donors is explored further then these four tenets are suggested as a guide: Tenet 1: the overarching principle is to appreciate and recognize the altruistic behavior of organ donors, and not the next of kin. Tenet 2: the second priority of reimbursing funeral expenses is to motivate the passive-positive public to sign up for organ donation. Tenet 3: the ultimate beneficiary from an incentive system is society, with an improved deceased organ donation rate. Government and charitable organizations, but not organ recipients, should be the source of payment. Tenet 4: as a token of expressing gratitude to the deceased organ donors, funeral expenses reimbursement preferably should be offered to those who have expressed the wish to donate (donor registration); they should have been provided the option to decline the offer."
Thursday, January 7, 2021
Vouchers for organ donation, by Kim, Li, and Xu in JET
There are now a number of ways in which an organ donation (or registration as an organ donor) can turn into a future priority for receiving an organ. Here's a paper from the January JET that looks at an overlapping generation model in which priority vouchers can be inherited by family members. The paper considers how, while this increases the incentive for the patriarch (or matriarch) of a family to register as a deceased donor, inheriting the voucher might reduce the incentive for descendants to donate, since they already have some priority on the deceased donor waiting list. The paper models how this can be avoided by giving inherited vouchers increased priority when the current recipient registers.
Organ donation with vouchers by Jaehong Kim, Mengling Li, and Menghan Xu, Journal of Economic Theory, Volume 191, January 2021, https://doi.org/10.1016/j.jet.2020.105159
Abstract: The ever-increasing shortage of organs for transplantation has motivated many innovative policies to promote the supply of organs. This paper proposes and analyzes a general class of deceased organ allocation policies that assign priority on organ waiting lists to voucher holders to promote deceased donor registration. Priority vouchers can be obtained by self-registering for donation or through family inheritance. In an overlapping generations framework, we find that extending the donor priority benefits to future generations can improve the aggregate donation rate and social welfare. In particular, giving higher priority to voucher inheritors who register for donation is always beneficial regardless of the levels of population growth and care for future generations. By contrast, the efficacy of granting priority to nondonors with inherited vouchers depends on these two sociodemographic factors because of potential free-riding incentives.
***********
Related post:
Monday, September 26, 2016
Thursday, September 2, 2010
Organ Allocation Policy and the Decision to Donate
Kessler, Judd B. and Alvin E. Roth, Organ Allocation Policy and the Decision to Donate," June 2010. (As an added bonus, Judd is on the jobmarket this year.)
Here's the abstract: "Organ donations from deceased donors (cadavers) provide the majority of transplanted organs in the United States, and one deceased donor can save numerous lives by providing multiple organs. Nevertheless, most Americans are not registered organ donors despite the relative ease of becoming one. We study in the laboratory an experimental game modeled on the decision to register as an organ donor, and investigate a variety of strategies for increasing the donation rate. We find that an organ allocation policy giving priority on waiting lists to those who previously registered as donors has a significant positive impact on registration.
And this is from the concluding section
"Before further considering the benefits of the priority rule, it is worth noting that there are other ways to change policy that could positively affect the number of registered organ donors. For example, one proposal that has received a good deal of attention would change the current “opt in” registration method used in the United States to an “opt out” system in which everyone is presumed to be a donor unless he or she actively indicates otherwiseAnother proposal, “mandated choice” would require everyone (e.g. who applies for a driver’s license) to specifically indicate whether they wished to be a donor or not. We want to briefly argue here that the priority rule that we consider may create a more direct link between registration as an organ donor and subsequent successful organ recovery and transplantation than policies that change the procedure by which individuals register as organ donors.
Tuesday, December 14, 2010
Misc. organ transplant links: poetry and priority
All those organ recipients from one donor made me thing of this kidney transplant poem that (along with others by the same author) is reported by the Los Angeles Examiner: Los Angeles Poet G. Murray Thomas, an essential voice in a city where noone is ever doubting Thomas (HT gtaniwaki )
“YOUR KIDNEY JUST ARRIVED AT LAX”
"The doctor told me as I lay in pre-op prep.
I envisioned a special chartered flight,
an entire airplane filled with organs.
"Hearts with little heart shaped carry-ons.
They always watch the inflight movie
and cry all the way through.
"Livers splurging on one last drink;
they don’t think they’ll be allowed
where they’re going.
"The lungs eye the spot
where the oxygen masks drop.
"Corneas stare out at the passing countryside;
they always get a window seat.
"The spleens are always complaining
about security
about the length of the flight
about the lack of leg room
(although they have no legs).
"The gall bladder always gets in line
before his row is called.
"And there’s my kidney,
no doubt reading a book to pass the time
something classic: As I Lay Dying,
or Great Expectations,
or The Stranger.
"All of them wondering
about the journey ahead,
about their new home,
about their new life."
-G Murray Thomas
In other news, the Israeli priority rule is going into effect: Registered donors to get preference if they need organ
"...the Health Ministry’s Israel Transplant will “give priority” in the receipt of organs to people who previously signed an ADI card and gave consent to donate organs after their deaths.
"Their immediate family members will also be entitled to this benefit.
"The new policy, which is being promoted by a twoweek media campaign that began on Sunday, is aimed at narrowing the gap between the 10 percent of Israelis who are registered as potential donors with ADI and the 62% who, when polled, said they were willing to donate lifesaving organs after they die.
"The 2008 organ transplant law included a unique section that gives priority to ADI card holders and their immediate relatives who need a transplant organ. However, due to the need for many technical and other preparations, it has taken more than two years to launch the new policy, which was approved by a majority of experts.
"Anyone already registered with ADI or who signs up before December 31, 2011 will be entitled to the priority benefit starting on January 1, 2012, while anyone joining after December 31, 2011 will be entitled to the benefit from three years after the date of signing, according to Israel Transplant, which is chaired by Rambam Medical Center director-general Prof. Rafael Beyar.
"Tamar Ashkenazi, Israel Transplant’s long-time coordinator, said that she hopes the “bonus” will induce hundreds of thousands of people – from the age of 17 – to register with ADI as potential organ donors. Today, only 547,000 people, or 10% of the population of the requisite age, are registered. ADI is an organization named for Adi Ben-Dror, who died decades ago from the lack of a donor kidney.
"Ashkenazi noted that there are two computerized lists of people who need organ transplants, one of those in hospital who urgently need an organ and the other living at home who need one less urgently. Having an ADI card would give “additional points” that are allocated and, through computers, automatically calculate who is most suited for a specific organ among those of a compatible blood type. “The extra points will be a significant addition to those who urgently need an organ,” she said.
"For a few weeks after the media campaign ends, stands will remain in public places for signing up new ADI members."
Tuesday, January 24, 2017
Lifesharers has shut down:
(see my post from 2008: Tuesday, December 23, 2008 Lifesharers: organ donation as a club good rather than a public good
Here's the lifesharers final anouncment:
Monday, March 21, 2016
"If your durable power of attorney for healthcare mentions your agreement to donate your organs through LifeSharers, you should change it.
If you have told your family and/or your doctors that you want to donate your organs through LifeSharers, you should let them know that's no longer possible."
Judd Kessler and I proposed a model which distinguished between the effective Israeli approach and the well-intentioned but inefficacious Lifesharers approach as follows. In Israel, those who register for donation gain priority for the already existing pool of deceased donors, while in Lifesharers the initial members only gain priority for each other. So, if there is even a small cost of joining, there is an equilibrium at which no one joins lifesharers, and indeed, unfortunately, it seems that Lifesharers never gained enough members to facilitate even a single transplant.
Contrast the difficulty of getting mutual donation going (with each death leading to only a very low probability of making a donation possible), with the easier task faced by the 19 Century Society for Mutual Autopsy
Thursday, July 5, 2012
Priority for _live_ organ donation in Israel
Saturday, July 27, 2024
An Experimental Study of the Chinese Organ Allocation System
China presently has a low rate of organ donations per million population, so there's a lot of room for growth. Here's a study suggesting that giving priority on the waiting list to family members of donors could help (as it has done in Israel):
Li, Danyang, Luo, Jun, Ye, Hang and Zheng, Heng. "Is Family-Priority Rule the Right Path? An Experimental Study of the Chinese Organ Allocation System" The B.E. Journal of Economic Analysis & Policy, vol. 24, no. 3, 2024, pp. 929-964. https://doi-org.stanford.idm.oclc.org/10.1515/bejeap-2023-0213
Abstract: China is experiencing an organ shortage crisis. We experimentally test the effectiveness of the family-priority allocation rule on organ donation and argue that such incentive would be highly motivating in Chinese family-oriented culture. Results of our experiment show that introducing the family-priority rule can not only increase donor registration but also promote family consent. Such priority rule would be particularly effective to increase deceased organ donation in China, as it will significantly promote donor registration and meanwhile generate a consistent higher family consent rate in a more family-orientated culture.
Monday, September 26, 2016
The effects of Israel's new organ transplantation law on family consent for deceased donation
Incentivizing Authorization for Deceased Organ Donation With Organ Allocation Priority: The First 5 Years
by A. Stoler, J. B. Kessler, T. Ashkenazi, A. E. Roth, J. Lavee
American Journal of Transplantation, Volume 16, Issue 9, September 2016
Pages 2639–2645
Abstract
The allocation system of donor organs for transplantation may affect their scarcity. In 2008, Israel's Parliament passed the Organ Transplantation Law, which grants priority on waiting lists for transplants to candidates who are first-degree relatives of deceased organ donors or who previously registered as organ donors themselves. Several public campaigns have advertised the existence of the law since November 2010. We evaluated the effect of the law using all deceased donation requests made in Israel during the period 1998–2015. We use logistic regression to compare the authorization rates of the donors’ next of kin in the periods before (1998–2010) and after (2011–2015) the public was made aware of the law. The authorization rate for donation in the period after awareness was substantially higher (55.1% vs. 45.0%, odds ratio [OR] 1.43, p = 0.0003) and reached an all-time high rate of 60.2% in 2015. This increase was mainly due to an increase in the authorization rate of next of kin of unregistered donors (51.1% vs. 42.2%). We also found that the likelihood of next-of-kin authorization for donation was approximately twice as high when the deceased relative was a registered donor rather than unregistered (89.4% vs. 44.6%, OR 14.27, p < 0.0001). We concluded that the priority law is associated with an increased authorization rate for organ donation.
Monday, October 4, 2021
More on the UAE-Israel kidney exchange
If you're just tuning in, you can follow the story of the kidney exchange between the UAE and Israel here. The pairs who exchanged kidneys were an Israeli Arab husband and wife, a Jewish Israeli mother and daughter, and a mother and daughter who wish to be identified only as Arab residents of the United Arab Emirates. (I joined their family at their home for a meal when I was in Abu Dhabi, but won't say more about them.)
It isn't a surprise that the donor in each pair couldn't donate to the intended recipient, because in each pair the recipient was a highly sensitized mother ( i.e. for whom it was hard to find a compatible kidney, because she had many antibodies against human proteins). During childbirth, mothers can develop such antibodies to the father's proteins that the children inherited. So the father and the daughters were incompatible donors, since the mother had antibodies against the paternal proteins (human leukocyte antigens) in their kidneys. Together with the fact that the mothers were quite hard to match, and that Israel and the UAE are both small, each with populations of around ten million, they had to look across national borders.
Cross border kidney exchange requires some diplomacy, particularly when the countries involved are getting together for the first time (and don't necessarily have a long history of cooperation). The key medical diplomats were Dr. Tamar Ashkenazi* the director of Israel Transplant and Dr Ali Abdulkareem Al Obaidli, Chairman of the UAE National Transplant Committee. (Other key collaborators in the complicated logistics were Itai Ashlagi at Stanford and Atul Agnihotri and Mike Rees of the Alliance for Paired Kidney Donation.)
So this was the plan:
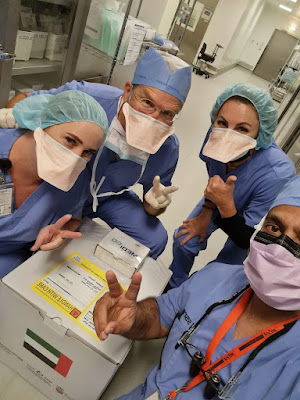
And here's a picture of the Abu Dhabi kidney packed for shipping (masked in the picture are Sue and Mike Rees, who have a lot of experience with packing and shipping kidneys, another nurse whose name I don't know, and Dr. Muhammad Badar Zaman the UAE transplant surgeon who transplanted the kidney that was on the way.
The little box taped to the top of the shipping container allows the kidney to be tracked in transit, via an app that gives you a picture of where it is at it travels:
And here's the swap of the two kidneys in shipping containers in the airport in Abu Dhabi (Tamar Ashkenazi and Dr. Ali are in the center, Atul and Mike are at the two ends...). Dr Ashkenazi was on both legs of the flight above--she flew in with the Israeli kidney and flew out with the UAE kidney.
On my last night in Abu Dhabi I had dinner with a lot of the docs. Across from me in the picture below are the two surgeons most actively involved in this exchange on the UAE side, transplant surgeon Dr. Zaman and the nephrectomy surgeon Dr. Hamid Reza Toussi. Next to me is the nephrologist Dr. Mohamed Yahya Seiari.
Tuesday, July 31, 2012
Priority for organ donation in the UK?
Britain's National Health Service is conducting a survey as part of an assessment of possible changes to its methods of acquiring and allocating organs for transplantation.
NHS considers organ donation shakeup
"The survey asks whether the UK should follow Israel's lead and say that those who are on the organ donor register should get priority if they subsequently need a transplant. "It always seemed to me that fairness is quite a fundamental British value but we have never put that in the context of organ donation," Johnson said.
"The NHSBT survey asks about extending the recently introduced practice by which the Driver and Vehicle Licensing Centre "nudges" those renewing or updating licences into deciding whether they want to join the donor register to other documents, such as marriage applications or wills. Johnson floated using the new universal credit, the single payment for those seeking work or on low incomes."
The article also speaks of the shortage of deceased donor organs:
"About 1,000 people die in the UK each year because they do not get a transplant, according to NHSBT. Johnson said more people wanted to become donors but the transplant service could not use all the organs they donated. More than 500,000 people die in Britain each year, but only about 3,000 in circumstances where they could realistically become organ donors.
"The reality is you have to die in hospital, on a ventilator, also in the intensive care or emergency department. The number of people dying who are under the age of 75, which is where most of our donors come from, has dropped by about 15% in the last few years. The people who are dying therefore tend to be older, they tend to have more co-morbidity than the rest of the population and, like the rest of the population, they have a tendency to be fatter. Consequently there are a number of people who would like us to use their organs but their organs might not be suitable."
**************
Before we get too excited, note that it's a lot easier to consider changes than to enact them: see my 2008 post on attempts in Britain to move towards presumed consent for organ donation.
Regarding priority for organ donation, Judd Kessler and I have a paper coming out in the August AER:
Kessler, Judd B. and Alvin E. Roth, '' Organ Allocation Policy and the Decision to Donate,'' American Economic Review, forthcoming.
Tuesday, January 22, 2013
Organs and elections in Israel
לראשונה: עמדות החתמה לכרטיס אדי בקלפיות |
"This is a joint project invented by someone at the National Transplantation Center and approved by the Ministry of Health.
++++++++++++++++
Post-election update:
Assaf writes:
Saturday, December 31, 2016
NSF grant on collaborative kidney exchange: final report
Here is the link to the page on which you can find the report by searching for Federal Award ID Number 1061932 (that takes you to a page that has found the grant, and then you have to click on the number to get the report--your government dollars at work as we used to say:)
For some reason, the final report is missing many of the publications reported in the annual progress reports...but it gives an idea of what we were thinking when we began this leg of the work, and some of the different directions in which we were led.
A more comprehensive list of publications from this work in the period 2011-16 is below, I may have more to say about them in the future.
Thursday, June 14, 2012
Misc. further notes on transplantation and deceased donation in Israel
The phenomenon I wrote about yesterday, about gaming the system, will take a while to evaluate, since only in time will people who signed donor cards under the new law become potential donors.
Here's an experimental paper forthcoming in the August AER, reporting a lab experiment with such a prioritiy scheme in an abstract setting (but without a strategy set large enough to explore the kind of gaming described yesterday):
Kessler, Judd B. and Alvin E. Roth, '' Organ Allocation Policy and the Decision to Donate,'' American Economic Review, forthcoming.
Monday, July 25, 2011
More on deceased organ donation in Israel
"Health officials are worried that the Knesset will authorize changes to organ donor cards that would move certain people up the waiting list for transplants without increasing the overall number of transplants. The officials are putting the blame on religious groups.
"In the current format, a potential donor may condition a donation on the decision of a clergyman of the family's choice.
""But MK Otniel Schneller (Kadima ) has put forth a bill to be sent to the Knesset Constitution, Law and Justice Committee. The bill would amend Article 28 of the organ transplant law of May 2008. Potential donors would be able to specify a religious figure or rabbinical committee that would approve an organ donation after the person's death.
"Over the past year, changes have been made that allow the health authorities to give preference in the transplant waiting list to anyone who signs an organ donor card.
"Health officials suspect that the proposed legislation is part of an effort by religious groups to bypass the system. In effect, people who do not genuinely intend to donate organs would receive preferential treatment while on the waiting list for a transplant. Their religious patron would then veto the organ donation if the person dies.
"A senior source in the medical establishment says that "this proposal may significantly curtail organ transplants in Israel."
"The privilege of being moved up on the waiting list if one is a donor is meant to go into effect in January for everyone who signs the donor card by then. The privilege can be exercised only three years after signing the card.
...
"The tension between the rabbis and doctors over organ transplants dates to 1986, when the Chief Rabbinate demanded that a religious representative be present when determining brain death. Only in 2009 was legislation on brain death approved, after a compromise forged by Schneller. The law requires that brain death be determined by a medical committee and objective machine-based data.
"Still, the Chief Rabbinate refused to acknowledge that brain death is a condition that allows for organs to be donated and transplanted."
HT: Maya Bar Hillel and Assaf Romm