Monday, April 1, 2013
Organs and executed prisoners: Jay Lavee goes to Taiwan
The first is to this story in the Tapei Times:
"Two issues surrounding organ transplants in Taiwan were spotlighted by foreign experts and Taiwanese legislators: using executed prisoners as organ donors and post-transplant medication insured by the NHI.
Jacob Lavee, director of the heart transplant unit at Israel’s Sheba Medical Center, said he used to hold up Taiwan on various occasions as a prominent example of a nation that had stopped taking organs from executed prisoners, who are considered unwilling donors, until he regretfully discovered Taiwan had resumed using such organs two years ago.
"The Department of Health’s Bureau of Planning head Shih Chung-yuan (石崇原) said in response that “although there is no law banning the use of organs taken from executed prisoners, the government does not encourage it and has stopped soliciting organ donations in the prison.”
"Concerning the current lawless state of organ transplants performed abroad, Shih said that in 2009, an amendment to the Organ Transplant Act (人體器官移植條例) was proposed that would require all organ recipients, in Taiwan or abroad, to register with local authorities, but it was not passed.
Tien also called for stricter regulation for organ transplants performed abroad, saying that since the majority (88.6 percent) of Taiwanese organ recipients went to China for organ transplants that are often from questionable and unethical organ sources, but continue to be insured by the NHI for post-transplant medication, “it almost seems like all Taiwanese who contribute to the NHI are complicit with the illegal and unethical organ-harvesting crimes perpetrated in China.”
***********
Here's a related story from NTD news: Taiwan's Health Department Wants to Criminalize Organ Trade
Taiwan’s health department said on Thursday it plans to modify its organ transplant laws to criminalize organ trade and brokerage.
The main concern is illegally obtained organs in China, where authorities have been accused of killing prisoners of conscience for their organs. China is the main destination for Taiwanese patients who obtain organs overseas.
[Hsu Ming-neng, Director, Bureau of Medical Affairs, Department of Health]:
“We want to minimize the occurrence of using organs with questionable sources. We plan to discuss the amendment of organ transplant laws [during the upcoming legislative period] and we want everyone’s support.”
Hsu Ming-neng spoke during a forum in Taipei on Thursday organized by the Department of Health. On the panel was a group of five doctors and investigators from around the world. They visited Taiwan this week to highlight transplant abuse in China.
Dr Jacob Lavee from Israel discovered his patients were going to China for rapid transplants. Some were promised an organ on a certain day—something that suggests China has an “on-demand” organ supply.
He has since worked to get Israel to stop transplant tourism to China.
[Jacob Lavee, MD, Advisor, Doctors Against Forced Organ Harvesting]:
“Those brokers who intermediate between local candidates and overseas [donors in China], that should be taken care of. That’s what we’ve done in Israel and that’s the way we’ve succeeded in Israel to stop completely the flow of Israeli patients to China.”
US-based doctor, Jianchao Xu, says a combined effort is necessary to stop forced organ harvesting in China.
[Jianchao Xu, MD, Medical Director, Doctors Against Forced Organ Harvesting]:
“I think the public, medical community, the political field and the legal community all need to take action, because this isn’t something that doctors alone can accomplish.”
Independent investigators and human rights activists have accused the Chinese regime of profiting from forced organ harvesting. The largest groups of victims identified are persecuted Falun Gong practitioners. Detained House Christians and Uyghur minorities are also believed to be amongst those killed for their organs.
NTD News, Taiwan
Wednesday, July 3, 2019
Lay attitudes towards organ donation from executed prisoners--by Bar-Hillel and Lavee
Lay attitudes toward involuntary organ procurement from death-row prisoners: no, but
- MAYA BAR-HILLEL (a1) and JACOB LAVEE (a2)
- DOI: https://doi.org/10.1017/bpp.2019.16
- Published online: 25 June 2019
Saturday, August 24, 2013
Organ donation in Britain: will it follow Israel's lead?
Registered organ donors could be given priority for transplants
"Patients who have agreed to donate organs could be given priority if they ever need a transplant, under proposals being considered by the NHS.
...
"In a report published today (THURS) NHS Blood and Transplant published a new plan to improve organ donations.
"The report floats one approach where patients already on the Organ Donor Register would be given higher priority for transplants should they need one.
"Professor James Neuberger, associate medical director at NHS Blood and Transplant, said: “They do this in Israel and it has encouraged donation.
“It was first introduced in Singapore. While they don’t exclude those who don’t donate, it gives priority to those who are on the donor register.
“Whether it is appropriate for the UK is up for debate and discussion.”
"Any move to prioritise patients on the donor register would require a decision by ministers and a change in organ allocation rules."
******************
The subject will be debated at the upcoming National Donation and Transplantation Congress, which is being held at the University of Warwick in early September.
Here's the announcement of the debate, with Jay Lavee, the Israeli heart transplant surgeon who has been at the heart of the change to priority in Israel speaking in favor (and presumably some of the others speaking against...)
Here is the UK Organ Donation and Transplantation site, and here are some links to the NHS Blood and Transplant Service documents on current proposals:
Taking Organ Transplantation to 2020
 Here's the accompanying full report (pdf)
Here's the accompanying full report (pdf)The table is from that report, summarizing the goals and current situation.
Here are other earlier posts following Jay Lavee's work
Friday, June 3, 2022
Organ transplants and capital punishment don't go well together
I recently blogged about a paper by Robertson and Lavee in the American Journal of Transplantation, looking at surgeries conducted in China before 2015, a period in which China acknowledged that most transplants there were conducted with organs from executed prisoners. Now they summarize their report in a column in the WSJ.
In China, New Evidence That Surgeons Became Executioners. Clinical reports recount scores of cases in which organ donors were alive when operations began. By Jacob Lavee and Matthew P. Robertson
"The Wuhan doctors write: “When the chest of the donor was opened, the chest wall incision was pale and bloodless, and the heart was purple and beating weakly. But the heartbeat became strong immediately after tracheal intubation and oxygenation. The donor heart was extracted with an incision from the 4th intercostal sternum into the chest. . . . This incision is a good choice for field operation where the sternum cannot be sawed open without power.”
"By casually noting that the donor was connected to a ventilator (“tracheal intubation”) only at midsurgery, the physicians inadvertently reveal that the donor was alive when the operation began.
...
"Our findings end in 2015, but we think the abuse likely continues. Medical papers like those we studied were first unearthed by Chinese grass-roots investigators in late 2014, and it would have been simple to command journals to stop publishing the incriminating details after that. While China claims to have stopped using prisoners in 2015, our previous research raises doubts. In a 2019 paper in the journal BMC Medical Ethics, we used statistical forensics to show that the official voluntary-organ donation numbers were falsified, inflating the success of a modest voluntary organ-donation reform program used to buttress the reform narrative.
"Global medical leaders have largely dismissed such concerns. The World Health Organization took advice from Chinese transplant surgeons in the establishment of its anti-organ-trafficking task force—and then installed them on the membership committee. In 2020, WHO officials joined long-time apologists for China’s transplant system, attacking our previous research showing falsified numbers."
...
"Dr. Lavee is the director of the Heart Transplantation Unit at Tel Aviv’s Sheba Medical Center and a professor of surgery at Tel Aviv University. Mr. Robertson is a research fellow with the Victims of Communism Memorial Foundation and a doctoral candidate in political science at the Australian National University."
Thursday, October 25, 2012
Jay Lavee on organ transplantation policy in Israel
Wednesday, November 26, 2014
Jacob Lavee on preventing transplant tourism, in the birthplace of transplantation
Monday, October 4, 2021
More on the UAE-Israel kidney exchange
If you're just tuning in, you can follow the story of the kidney exchange between the UAE and Israel here. The pairs who exchanged kidneys were an Israeli Arab husband and wife, a Jewish Israeli mother and daughter, and a mother and daughter who wish to be identified only as Arab residents of the United Arab Emirates. (I joined their family at their home for a meal when I was in Abu Dhabi, but won't say more about them.)
It isn't a surprise that the donor in each pair couldn't donate to the intended recipient, because in each pair the recipient was a highly sensitized mother ( i.e. for whom it was hard to find a compatible kidney, because she had many antibodies against human proteins). During childbirth, mothers can develop such antibodies to the father's proteins that the children inherited. So the father and the daughters were incompatible donors, since the mother had antibodies against the paternal proteins (human leukocyte antigens) in their kidneys. Together with the fact that the mothers were quite hard to match, and that Israel and the UAE are both small, each with populations of around ten million, they had to look across national borders.
Cross border kidney exchange requires some diplomacy, particularly when the countries involved are getting together for the first time (and don't necessarily have a long history of cooperation). The key medical diplomats were Dr. Tamar Ashkenazi* the director of Israel Transplant and Dr Ali Abdulkareem Al Obaidli, Chairman of the UAE National Transplant Committee. (Other key collaborators in the complicated logistics were Itai Ashlagi at Stanford and Atul Agnihotri and Mike Rees of the Alliance for Paired Kidney Donation.)
So this was the plan:
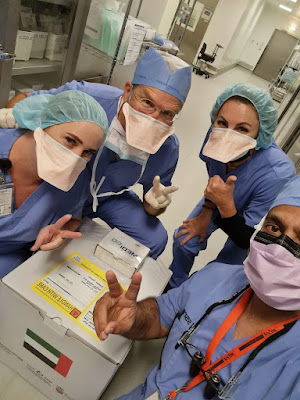
And here's a picture of the Abu Dhabi kidney packed for shipping (masked in the picture are Sue and Mike Rees, who have a lot of experience with packing and shipping kidneys, another nurse whose name I don't know, and Dr. Muhammad Badar Zaman the UAE transplant surgeon who transplanted the kidney that was on the way.
The little box taped to the top of the shipping container allows the kidney to be tracked in transit, via an app that gives you a picture of where it is at it travels:
And here's the swap of the two kidneys in shipping containers in the airport in Abu Dhabi (Tamar Ashkenazi and Dr. Ali are in the center, Atul and Mike are at the two ends...). Dr Ashkenazi was on both legs of the flight above--she flew in with the Israeli kidney and flew out with the UAE kidney.
On my last night in Abu Dhabi I had dinner with a lot of the docs. Across from me in the picture below are the two surgeons most actively involved in this exchange on the UAE side, transplant surgeon Dr. Zaman and the nephrectomy surgeon Dr. Hamid Reza Toussi. Next to me is the nephrologist Dr. Mohamed Yahya Seiari.
Tuesday, March 19, 2024
The Impact of prioritization on kidney and liver allocation in Israel
Israel's Organ Transplantation Law grants some priority on waiting lists for transplants to candidates who are first-degree relatives of deceased organ donors (i.e. whose family has given permission for someone's deceased organ donation) or who previously registered as organ donors themselves. (There's also a tiny priority for relatives of people who signed organ donor cards...) Here are two papers that looks at the effect of those priorities on kidney and liver transplants, and how they interact with other priorities on waiting lists for Israeli organs.
The first paper, on kidneys, concludes that the priorities are effective in reducing waiting time to transplant, and suggests that perhaps these priorities should not be so large compared to other existing priorities (e.g. for time on dialysis), or for priorities that could be established, e.g. for highly sensitized patients (who get high priority in the U.S., for example.)
Mor, Eytan, Meitar Bloom, Ronen Ghinea, Roi Anteby, Ronit Pasvolsky-Gutman, Ron Loewenthal, Ido Nachmani, and Tammy Hod. "The Impact of the Donor Card Holder Prioritization Program on Kidney Allocation in Israel." Transplantation (2024): 10-1097.
Abstract
Background: Since 2014, as part of a priority program within the Israeli Transplant Law, additional points were given to waitlisted candidates with donor cards. We assessed the impact on deceased donor kidney allocation.
Methods: This study enrolled all patients older than 18 y who underwent deceased donor kidney transplantation (January 2016–December 2019). Data were obtained from the National HLA Tissue Laboratory registry at the Sheba Medical Center. Patients were grouped by donor card status (ADI group) (not signed, 0 points; relative signed, 0.1 points; patient signed, 2 points; and relative donated, 9 points). The primary outcome was waiting time until kidney transplantation with and without the additional score.
Results: Four hundred forty-four patients underwent kidney transplantation during the study period: 281 (63%) were donor card holders (DCH) and 163 (37%) were not DCH. DCH with extra points waited 68.0 (±47.0) mo on average, compared with 94.6 (±47.3) mo for not DCH (P < 0.001). Donor card signers had a shorter time until transplant in a multivariable model. Without extra points, 145 recipients (32.6%) would have missed organs allocated to higher-scored candidates. Allocation changes occurred in 1 patient because of an additional 0.1 points, in 103 candidates because of an additional 2 points, and in 41 candidates because of an additional 9 points.
Conclusions: Additional DCH scores improved allocation and reduced waiting time for donor card signers and those with donating relatives. To enhance fairness, consideration should be given to reducing the score weight of this social criterion and raising scores for other factors, especially dialysis duration.
##########
There are many fewer liver transplants than kidney transplants, and the effect of priority is less clear:
Ashkenazi, Tamar, Avraham Stoler, and Eytan Mor. "The effect of priority given to donor card holders on the allocation of livers for transplant—evidence from 7 years of the Israeli priority program." Transplantation 106, no. 2 (2022): 299-307.
Abstract
Background. The Israeli Transplant Law grants priority in organ allocation to patients signing a donor card. Liver transplant candidates get additional 2 points on their Model for End Stage Liver Disease score for signing a donor card, 0.1 points for a relative holding a card, and 5 points if a relative donated an organ. We studied the effect of the priority program on waiting list mortality and allocation changes due to priority.
Methods. Using Israeli Transplant data of 531 adult liver transplant candidates with chronic liver disease listed between 2012 and 2018 we compared waitlist mortality and transplant rate of candidates with and without priority. Then we analyzed liver allocations resulting from additional priority points and followed outcome of patients who were skipped in line.
Results. Of the 519 candidates, 294 did not sign a donor card, 82 signed, 140 had a relative sign, and for 3, a relative donated an organ. The rates of waitlist mortality in these 4 groups were 22.4%, 0%, 21.4%, and 0%, respectively, and the transplant rates were 50%, 59.8%, 49.3%, and 100%, respectively. Of the 30 patients who were skipped because of priority, 24 subsequently underwent transplant, 2 are on the waiting list, and 4 died within 0.75, 1.75, 7, and 17 mo.
Conclusions. The 2 points added to the Model for End Stage Liver Disease score were associated with lower waitlist mortality and higher transplant rate for candidates signing a donor card without significantly affecting access to transplant during allocation. Further research and consideration of optimal policy when granting priority for candidates signing a donor card should continue.
###########
Earlier:
Stoler, Avraham, Judd B. Kessler, Tamar Ashkenazi, Alvin E. Roth, Jacob Lavee, “Incentivizing Authorization for Deceased Organ Donation with Organ Allocation Priority: the First Five Years,” American Journal of Transplantation, Volume 16, Issue 9, September 2016, 2639–2645.
Stoler, Avraham, Judd B. Kessler, Tamar Ashkenazi, Alvin E. Roth, Jacob Lavee, “Incentivizing Organ Donor Registrations with Organ Allocation Priority,”, Health Economics, April 2016 Volume: 26 Issue: 4 Pages: 500-510 APR 2017
Saturday, December 31, 2016
NSF grant on collaborative kidney exchange: final report
Here is the link to the page on which you can find the report by searching for Federal Award ID Number 1061932 (that takes you to a page that has found the grant, and then you have to click on the number to get the report--your government dollars at work as we used to say:)
For some reason, the final report is missing many of the publications reported in the annual progress reports...but it gives an idea of what we were thinking when we began this leg of the work, and some of the different directions in which we were led.
A more comprehensive list of publications from this work in the period 2011-16 is below, I may have more to say about them in the future.
Monday, January 27, 2014
New transplant statistics from Israel
"Last year brought good news to the Israel Transplant Center and to 392 people whose lives were saved by deceased and live donors.
There was an increase by 24 percent of live kidney donors; 56% of family members of deceased agreed to donate organs; 90,000 more people signed donor cards; and almost half of those who received organs from deceased donors were advanced in the queue because they had signed a donor card.
In addition, the first transplant of a small intestine was successfully performed and 637 corneas were also transplanted in 769 patients (some were split into parts), giving recipients the gift of sight, the center announced on Sunday.
Of the 143 requests to families whose loved ones suffered lower-brain death, 80 of them consented to give one or more organs. The families said it was important to save the lives of others, while the most common reason for refusal were “religious” – even though modern Orthodox clergymen say donating fulfills a very important positive commandment – and the concern that the body to be buried would “not be whole.”
The figure of 392 donated organs was the highest ever.
Of these, 104 of the donors were from live relatives (who gave a kidney or liver lobe), and the rest were from altruistic families who gave their loves ones’ organs.
Of 248 organs from deceased donors, 109 of the recipients had to wait less because they had previously signed up as potential donors. The number of patients waiting to receive a lifesaving organ dropped from 1,114 in 2012 to 1,075 in 2013.
Of the 109 recipients who were advanced in the queue, four received hearts, 25 received lungs, 13 received livers and 67 received kidneys.
Of the deceased donors, 112 were donors of kidneys, 10 of kidney-pancreases, 5 double kidneys (usually from elderly donors), 57 of livers, one liver and kidney, 13 hearts, 24 double lungs, 25 single lungs and one “domino” donation of a liver (when an organ or part of one is removed for the primary purpose of a person’s medical treatment and may prove suitable for transplant into another person)."
HT: Jay Lavee
Thursday, January 16, 2014
Organ donor registration in Israel
*******************
The work Jay is referring to is a paper, currently out for review at a journal that doesn't like prepublication on the web, "Don’t Take ‘No’ For An Answer: An experiment with actual organ donor registrations," which finds, in a study of the online MA state organ donor registry, that requiring potential donors to choose either "yes" or "no" when asked if they wish to be on the donor registry does not increase registrations, and seems likely to reduce the rate of donations by next of kin when the deceased is unregistered.
Sunday, March 31, 2013
Organs and Inducements at Duke
 |
| Judd Kessler, Jay Lavee, Al Roth, Avi Stoler |
Kim Krawiec posts about the conference at the Faculty Lounge: I reproduce her post below...
"Organs & Inducements
Update: here's a further post today by Kim K., on the origins of the conference (and why they chose the word "inducements" rather than "incentives": More Organs & InducementsSymposium Abstract:The need for human organs for transplantation far outstrips supply. As a result, a large literature has developed debating possible means to address the gap. Suggestions range from procurement system improvements and changes in the consent regime, in the case of cadaveric organ donation, to inventive exchange systems (such as swaps and NEAD chains) and financial incentives of various sorts, in the case of live organ donation.In Organs and Inducements, contributors build on existing debates on mechanisms designed to bridge the gap between organ demand and supply, to address deeper questions regarding inducements to donate. Among the varied possible mechanisms of persuasion and incentives at society’s disposal, what are the relative advantages and disadvantages of each? What are the larger ethical, economic, sociological, and psychological issues raised by these different types of inducements, including non-financial inducements? Why are some accepted by the law and society at large, while others are not? Do the lines we’ve drawn among permissible and impermissible inducements make sense, given the concerns those rules are meant to address?"*************************************************
Saturday, April 9, 2022
"Execution by organ procurement: Breaching the dead donor rule in China," by Matthew P. Robertson, and Jacob Lavee in the AJT
Prior to 2015, it was legal in China to transplant organs recovered from executed prisoners. When I visited China in those days to talk about kidney transplantation from living donors, it was sometimes pointed out to me that, as an American, I shouldn't object to the Chinese use of executed prisoner organs, because we also had capital punishment in the US, but we "wasted the organs." I replied that in the US we had both capital punishment and transplantation, but were trying to limit one and increase the other, and that I didn’t think that either would be improved by linking it to the other.
So here's a just-published retrospective paper looking at Chinese language transplant reports prior to 2015, which identifies at least some instances that it regards as "execution completed by organ procurement."
Execution by organ procurement: Breaching the dead donor rule in China, by Matthew P. Robertson1, and Jacob Lavee2, American Journal of Transplantation, Early View, First published: 04 April 2022 https://doi.org/10.1111/ajt.16969
1 Australian National University | Victims of Communism Memorial Foundation, Washington, D.C., USA
2 Heart Transplantation Unit, Leviev Cardiothoracic Center, Sheba Medical Center, Faculty of Medicine, Tel Aviv University, Ramat Gan, Israel
Abstract: The dead donor rule is fundamental to transplant ethics. The rule states that organ procurement must not commence until the donor is both dead and formally pronounced so, and by the same token, that procurement of organs must not cause the death of the donor. In a separate area of medical practice, there has been intense controversy around the participation of physicians in the execution of capital prisoners. These two apparently disparate topics converge in a unique case: the intimate involvement of transplant surgeons in China in the execution of prisoners via the procurement of organs. We use computational text analysis to conduct a forensic review of 2838 papers drawn from a dataset of 124 770 Chinese-language transplant publications. Our algorithm searched for evidence of problematic declarations of brain death during organ procurement. We find evidence in 71 of these reports, spread nationwide, that brain death could not have properly been declared. In these cases, the removal of the heart during organ procurement must have been the proximate cause of the donor's death. Because these organ donors could only have been prisoners, our findings strongly suggest that physicians in the People's Republic of China have participated in executions by organ removal.
"how should we understand the physician's role in a context where executed prisoners are the primary source of transplant organs? Might the transplant surgeon become the de facto executioner? Evidence suggestive of such behavior has emerged over many years from the People's Republic of China (PRC).8-14 To investigate these reports, this paper uses computational methods to examine 2838 Chinese transplant-related medical papers published in scientific journals, systematically collecting data and testing hypotheses about this practice. By scrutinizing the clinical procedures around intubation and ventilation of donors, declaration of brain death, and commencement of organ procurement surgery, we contribute substantial new evidence to questions about the role of PRC physicians in state executions.
...
"The data we rely on in this paper involves transplant surgeries from 1980 to 2015. During this period, there was no voluntary donation system and very few voluntary donors. According to three official sources, including the current leader of the transplant sector, the number of voluntary (i.e., non-prisoner) organ donors in China cumulatively as of 2009 was either 120 or 130,30-32 representing only about 0.3% of the 120 000 organs officially reported to be transplanted during the same period (on the assumption that each voluntary donor gave three organs).18, 33, 34 The leader of China's transplant sector wrote in 2007 that effectively 95% of all organ transplants were from prisoners.35 According to official statements, it was only in 2014 that a national organ allocation system could be used by citizens.36
...
"Procuring vital organs from prisoners demands close cooperation between the executioner and the transplant team. The state's role is to administer death, while the physician's role is to procure a viable organ. If the execution is carried out without heed to the clinical demands of the transplant, the organs may be spoiled. Yet if the transplant team becomes too involved, they risk becoming the executioners.
"Our concern is whether the transplant surgeons establish first that the prisoners are dead before procuring their hearts and lungs. This translates into two empirical questions: (1) Is the donor intubated only after they are pronounced brain dead? And (2) Is the donor intubated by the procurement team as part of the procurement operation? If either were affirmative the declaration of brain death could not have met internationally accepted standards because brain death can only be determined on a fully ventilated patient. Rather, the cause of death would have been organ procurement.
...
"We define as problematic any BDD in which the report states that the donor was intubated after the declaration of brain death, and/or the donor was intubated immediately before organ procurement, as part of the procurement operation, or the donor was ventilated by face mask only.
...
"The number of studies with descriptions of problematic BDD was 71, published between 1980 and 2015. Problematic BDD occurred at 56 hospitals (of which 12 were military) in 33 cities across 15 provinces.
...
"We have documented 71 descriptions of problematic brain death declaration prior to heart and lung procurement. From these reports, we infer that violations of the DDR took place: given that the donors could not have been brain dead before organ procurement, the declaration of brain death could not have been medically sound. It follows that in these cases death must have been caused by the surgeons procuring the organ.
"The 71 papers we identify almost certainly involved breaches of the DDR because in each case the surgery, as described, precluded a legitimate determination of brain death, an essential part of which is the performance of the apnea test, which in turn necessitates an intubated and ventilated patient. In the cases where a face mask was used instead of intubation48, 49—or a rapid tracheotomy was followed immediately by intubation,50 or where intubation took place after sternal incision as surgeons examined the beating heart44—the lack of prior determination of brain death is even more apparent.
"If indeed these papers document breaches of the DDR during organ procurement from prisoners as we argue, how were these donors prepared for organ procurement? The textual data in the cases we examine is silent on the matter. Taiwan is the only other country we are aware of where death penalty prisoners’ vital organs have been used following execution. This reportedly took place both during the 1990s and then once more in March 2011.51, 52
...
"The PRC papers we have identified do not describe how the donor was incapacitated before procurement, and the data is consistent with multiple plausible scenarios. These range from a bullet to the prisoner's head at an execution site before they are rushed to the hospital, like Tsai's description, or a general anesthetic delivered in the operating room directly before procurement. Paul et al. have previously proposed a hybrid of these scenarios to explain PRC transplant activity: a lethal injection, with execution completed by organ procurement.
...
"We think that our failure to identify more DDR violations relates to the difficulty of detecting them in the first instance, not to the absence of actual DDR violations in either the literature or practice. Our choice to tightly focus only on papers that made explicit reports of apparent DDR violations likely limited the number of problematic papers we ultimately identified.
...
"As of 2021, China's organ transplant professionals have improved their reputation with their international peers. This is principally based on their claims to have ceased the use of prisoners as organ donors in 2015."
Monday, July 27, 2009
Corruption and kidneys in New Jersey and Brooklyn
Almost as an aside, the story reports that a broker for transplant kidneys was caught in the net:
"Another man in Brooklyn, Levy-Izhak Rosenbaum, was accused of enticing vulnerable people to give up a kidney for $10,000 and then selling the organ for $160,000. Mr. Dwek pretended to be soliciting a kidney on behalf of someone and Mr. Rosenbaum said that he had been in business of buying organs for years, according to the complaint."
Part of the repugnance to the transaction seems to be the buying and selling prices. (Would we/should we feel differently if the kidneys were bought for $100,000 and sold for $115,000?)
Steve Leider points me to an Indiana Jones connection: Anthropologist's 'Dick Tracy moment' plays role in arrest of suspected kidney trafficker. (The anthropologist in question, Nancy Scheper-Hughes, writes frequently about black markets for kidneys, and apparently indentified Mr Rosenbaum some years ago, although the story doesn't suggest to me an immediate connection to the recent arrest.)
Parag Pathak points me towards Benyamin Cohen's story in Slate, following up on the Jewish connection: The arrests of rabbis who trafficked body parts uncover more complicated issues, that suggests some of the nuances of Jewish religious jurisprudence about organ donation and sales.
Trying to figure out Jewish law directly from the Bible skips a couple of centuries of subsequent interpretation. Here's what I wrote about kidney sales in a footnote of my paper Repugnance as a constraint on markets:
3 While there is no central authority on the application of Jewish law to modern concerns such as transplantation, the most authoritative opinions are contained in various “responsa” or answers to particular questions by rabbis acting as legal “deciders” (poskim), whose authority arises from the respect of their peers. The consensus on the matter of live kidney donation, for example, seems to be that live donation is allowed (since it saves lives), but it is not required (since the donor becomes wounded and takes some risk to his own life), and hence it falls into the category of things for which compensation could be offered and accepted (unlike actions that are either forbidden or required). See, for example, Eisenberg (2006), Grazi and Wolowelsky (2004), Kunin (2005), and Israeli (1997) who cite eminent modern poskim such as Rabbi Shlomo Zalman Auerbach and Rabbi Moshe Feinstein."
"For example, Avraham (2004, p. 271–2) reports the opinion of the eminent Rabbi Shlomo Zalman Auerbach that someone who sells a kidney with the intention of saving a life does a good deed “even if he would not have donated his kidney only to save life.” But he goes on to note, “[I ]n spite of all that has been said above, it seems to me that it is the community that needs soul-searching for allowing a person to reach such a depth of despair that he must sell a kidney, either because of poverty, debts, or the inability to pay for a relative’s medical expenses.”
Although mainstream Jewish authorities support organ donation, some streams of ultra-orthodox Judaism do not: here's a disturbing article brought to my attention by Miran Epstein, from Yediot: Heart recipient's father: We'll never donate organs
It goes on to note
"The father's words angered Prof. Yaacov Lavee, director of the Heart Transplantation Unit at the Sheba Medical Center. "This is outrageous," he said. "I've heard such statements from many of my candidates (for a transplant), who weren't ashamed to admit they wouldn't donate organs.
"Such statements led me to initiate the bill that prioritizes transplants for people who have signed an organ donor card. This is clearly immoral behavior," he added.
The new transplant law, which will go into effect in May, states that any person in need of a transplant and who has had an organ donor card for at least three years will be given priority on the organ transplant waiting list. "
This makes some aspects of Israeli transplant law resemble parts of Singapore's transplant law, which also gives priority for organs to those who are registered as donors. (I wrote about this near the end of an earlier post.)
Update: Sally Satel's take is in the WSJ: About That New Jersey Organ Scandal It’s not surprising when 80,000 Americans are waiting for kidneys, and a background piece from Time magazine: How Does Kidney-Trafficking Work?