Tuesday, February 15, 2011
Two faces of kidney transplantation
One is the great Boston College economist Tayfun Sonmez, one of the pioneers of kidney exchange.
The other is the (also) Turkish kidney transplant surgeon Yusuf Sonmez, who is once again in the news for his alleged role in both kidney black markets and in war crimes in Kosovo. In a recent interview in the NY Times, focusing primarily on the black market allegations, he is asked about both the recipients and the donor/vendors: Monster or Savior? Doctor Draws New Scrutiny.
“There are two Yusufs, one my family and friends know and the one created in the press who is a monster— this is a drama, a tragedy,” said Dr. Sonmez, 53, a trim, angular man with intense, gray-green eyes and a graying goatee. “Up to now, I didn’t kill anybody. I didn’t harm anybody, counting donors or recipients. I have not committed any kind of social harm to anyone. This is the main thing that I am proud of.”
...
"Dr. Sonmez is wanted with regard to one of the most troubling prosecutions to emerge recently— a European Union investigation into trafficking in Kosovo in which seven people, mostly prominent local doctors, have been charged with illegal kidney transplants in a private clinic. Dr. Sonmez has not been charged in Kosovo, but the prosecution contends he played a central role in the ring.
"That case has become intertwined with a volatile two-year Council of Europe inquiry that made links between the Kosovo prime minister, Hashim Thaci, and a criminal enterprise of some former Kosovo Liberation Army fighters accused of executing Serbian prisoners in 1999 and 2000 for their organs.
"Dr. Sonmez has denied wrongdoing in either situation, but a Turkish immigrant who lost consciousness at an airport in Kosovo after a kidney removal, and the patient who investigators say received his kidney, both identified Dr. Sonmez as part of the operating team. He says he was only in the operating room offering advice to others.
"Investigators have focused on the role of Dr. Sonmez in 2008 as a surgeon for the Medicus private clinic in a rundown neighborhood in Pristina, Kosovo’s capital, where they said kidneys were removed from impoverished immigrants recruited on false promises of payment that they never received. The organs were transplanted to wealthy patients from Canada, Germany, Poland and Israel who paid up to €90,000, or $122,000.
...
"By his estimate, most of the thousands of transplants he has performed since he began in 1992 involved live, unrelated donors. He said his survival rate was high because he presided over the removal and transplant of kidneys, monitoring patients side by side for 48 hours.
“This is amazing,” he said of the transplant process. “I love it — to watch the changes with the new organ, the changes in the body, to move with the changes, to make changes in the medication.”
"Typically, he said, he requires donors and recipients to submit signed, notarized statements to declare that money has not been exchanged.
"How does he know that desperately poor kidney donors are not being exploited by a murky world of brokers, fixers and wealthy donors with lavish insurance?
“I don’t need to ask these questions,” he said, “because I do believe that people have their own authority over their own body. They are not stealing, they are not cheating. So this is the shame of the system. Not their shame.”
...
"In the next few weeks, Dr. Sonmez and his lawyer are poised to head to Kosovo to give his statements.
“They want information about bigger fish,” said Murat Sofuoglu, an old friend and lawyer for Mr. Sonmez, who has been shuttling between Istanbul and Pristina to negotiate terms for the doctor to give a statement to prosecutors.
“Not me,” Dr. Sonmez said, picking at a honey-drenched piece of baklava. “I am not the big fish.”
Thursday, November 7, 2019
Controversial markets, at Humboldt University
************
Tonight I'll also speak at an event organized by the Einstein Institute, concerning how changes in the current German transplant law could make kidney exchange practical in Germany.
Saturday, November 4, 2023
The EU proposes strengthening bans on compensating donors of Substances of Human Origin (SoHOs)--op-ed in VoxEU by Ockenfels and Roth
The EU has proposed a strengthening of European prohibitions against compensating donors of "substances of human origin" (SoHOs). Here's an op-ed in VoxEU considering how that might effect their supply.
Consequences of unpaid blood plasma donations, by Axel Ockenfels and Alvin Roth / 4 Nov 2023
"The European Commission is considering new ways to regulate the ‘substances of human origin’ – including blood, plasma, and cells – used in medical procedures from transfusions and transplants to assisted reproduction. This column argues that such legislation jeopardises the interests of both donors and recipients. While sympathetic to the intentions behind the proposals – which aim to ensure that donations are voluntary and to protect financially disadvantaged donors – the authors believe such rules overlook the effects on donors, on the supply of such substances, and on the health of those who need them.
"Largely unnoticed by the general public, the European Commission and the European Parliament’s Health Committee have been drafting new rules to regulate the use of ‘substances of human origin’ (SoHO), such as blood, plasma, and cells (Iraola 2023, European Parliament 2023). These substances are used in life-saving medical procedures ranging from transfusions and transplants to assisted reproduction. Central to this legislative initiative is the proposal to ban financial incentives for donors and to limit compensation to covering the actual costs incurred during the donation process. The goal is to ensure that donations are voluntary and altruistic. The initiative aims to protect the financially disadvantaged from undue pressure and prevent potential misrepresentation of medical histories due to financial incentives. While the intention is noble, the proposal warrants critical analysis as it may overlook the detrimental effects on donors themselves, on the overall supply of SoHOs, and consequently on the health, wellbeing, and even the lives of those who need them. We illustrate this in the context of blood plasma donation.
"Over half a century ago, Richard Titmuss (1971) conjectured that financial incentives to donate blood could compromise the safety and overall supply. This made sense in the 1970s, when tests for pathogens in the blood supply were not yet developed. But Titmuss’ conjecture permeated policy guidelines worldwide, despite mounting evidence to the contrary. Although more evidence is needed, a review published by Science (Lacetera et al. 2013; see also Macis and Lacetera 2008, Bowles 2016), which looked at the evidence available more than 40 years after Titmuss’ conjecture, concluded that the statistically sound, field-based evidence from large, representative samples is largely inconsistent with his predictions.
"Getting the facts right is important because, at least where blood plasma is concerned, the volunteer system has failed to meet demand (Slonim et al. 2014). There is a severe and growing global shortage of blood plasma. While many countries are unwilling to pay donors at home, they are willing to pay for blood plasma obtained from donors abroad. The US, which allows payment to plasma donors, is responsible for 70% of the world’s plasma supply and is also a major supplier to the EU, which must import about 40% of its total plasma needs. Together with other countries that allow some form of payment for plasma donations – including EU member states Germany, Austria, Hungary, and the Czech Republic – they account for nearly 90% of the total supply (Jaworski 2020, 2023). Based on what we know from controlled studies and from experiences with previous policy changes, a ban on paid donation in the EU will reduce the amount of plasma supplied from EU members, prompting further attempts to circumvent the regulation by importing even more plasma from countries where payment is legal. At the same time, a ban will contribute to the global shortage of plasma, further driving up the price and making it increasingly unaffordable for low-income countries (Asamoah-Akuoko et al. 2023). In the 1970s, it may have been reasonable to worry that encouraging paid donation would lead to a flow of blood plasma from poor nations to rich ones. That is not what we are in fact seeing. Instead, plasma supplies from the US and Europe save lives around the world.
"In other areas, society generally recognises the need for fair compensation for services provided, especially when they involve discomfort or risk. After all, it is no fun having someone stick a needle in your arm to extract blood. This consensus cuts across a range of services and professions – including nursing, firefighting, and mining – occupations, most people would agree, that should be well rewarded for the risk involved and value to society. To rely solely on altruism in such areas would be exploitative and would eventually lead to a collapse in provision. Indeed, to protect individuals from exploitation, labour laws around the world have introduced minimum compensation requirements rather than caps on earnings. In addition, payment bans on donors, even if they’re intended to protect against undue inducements, raise concerns about price-fixing to the benefit of non-donors in the blood plasma market. In a related case, limits on payment to egg donors have been successfully challenged in US courts. 1
"In addition, policy decisions affecting vital supplies such as blood plasma should be based on a broad discourse that includes diverse perspectives and motivations. Ethical judgements often differ, both among experts and between professionals and the general public, so communication is essential (e.g. Roth and Wang 2020, Ambuehl and Ockenfels 2017). Payment for blood plasma donations is an example. We (the authors of this article) are from the US and Germany, countries that currently allow payment for blood plasma donations while most other countries prohibit payment. On the other hand, prostitution is legal in Germany but surrogacy is not, while the opposite is true in most of the US. And while Germany currently prohibits kidney exchange on ethical grounds, other countries – including the US, the UK, and the Netherlands – operate some of the largest kidney exchanges in the world and promote kidney exchange on ethical grounds.
"The general public does not always share the sentiments that health professionals find important (e.g. Lacetera et al. 2016). This tendency is probably not due to professionals being less cognitively biased. In all areas where the question has been studied, experts such as financial advisers, CEOs, elected politicians, economists, philosophers, and doctors are just as susceptible to cognitive bias as ordinary citizens (e.g. Ambuehl et al. 2021, 2023). Recognising the similarities and differences between professional and popular judgements, and how ethical judgements are affected by geography, time, and context, allows for a more constructive and effective search for the best policy options.
"In our view, the dangers of undersupply of critical medical substances, of inequitable compensation (particularly for financially disadvantaged donors), and of circumvention of regulation by sourcing these substances from other countries (where the EU has no influence on the rules for monitoring compensation to protect donors from harm) are at least as significant as those arising from overpayment. Carefully designed transactional mechanisms may also help to respect ethical boundaries while ensuring adequate supply. Advances in medical and communication technologies, such as viral detection tests, can effectively monitor blood quality and ensure the safety and integrity of the entire donation process – including the deferral of high-risk donors and those for whom donating is a risk to their health – without prohibiting payment to donors. Even if it is ultimately decided that payments should be banned, there are innovations in the rules governing blood donation that have been proposed, implemented, and tested that would improve the balance between blood supply and demand within the constraints of volunteerism; non-price signals, for instance, can work within current social and ethical constraints.
"As the EU deliberates on this legislation, it is imperative to adopt a balanced, empirically sound, and research-backed approach that considers multiple effects and promotes policies to safeguard the interests of both donors and recipients.
References
Asamoah-Akuoko, L et al. (2023), “The status of blood supply in sub-Saharan Africa: barriers and health impact”, The Lancet 402(10398): 274–76.
Ambuehl, S and A Ockenfels (2017), “The ethics of incentivizing the uninformed: A vignette study”, American Economic Review Papers & Proceedings 107(5), 91–95.
Ambuehl, S, A Ockenfels and A E Roth (2020), “Payment in challenge studies from an economics perspective”, Journal of Medical Ethics 46(12): 831–32.
Ambuehl, S, S Blesse, P Doerrenberg, C Feldhaus and A Ockenfels (2023), “Politicians’ social welfare criteria: An experiment with German legislators”, University of Cologne, working paper.
Ambuehl, S, D Bernheim and A Ockenfels (2021), “What motivates paternalism? An experimental study”, American Economic Review 111(3): 787–830.
Bowles S (2016), “Moral sentiments and material interests: When economic incentives crowd in social preferences”, VoxEU.org, 26 May.
European Parliament (2023), “Donations and treatments: new safety rules for substances of human origin”, press release, 12 September.
Iraola, M (2023), “EU Parliament approves text on donation of substances of human origin”, Euractiv, 12 September.
Jaworski, P (2020), “Bloody well pay them. The case for Voluntary Remunerated Plasma Collections”, Niskanen Center.
Jaworski, P (2023), “The E.U. Doesn’t Want People To Sell Their Plasma, and It Doesn’t Care How Many Patients That Hurts”, Reason, 20 September.
Lacetera, N, M Macis and R Slonim (2013), “Economic rewards to motivate blood donation”, Science 340(6135): 927–28.
Lacetera, N, M Macis and J Elias (2016), “Understanding moral repugnance: The case of the US market for kidney transplantation”, VoxEU.org, 15 October.
Macis M and N Lacetera (2008), “Incentives for altruism? The case of blood donations”, VoxEU.org, 4 November.
Roth, A E (2007), “Repugnance as a constraint on markets”, Journal of Economic Perspectives 21(3): 37–58.
Roth A E and S W Wang (2020), “Popular repugnance contrasts with legal bans on controversial markets”, Proc Natl Acad Sci USA 117(33): 19792–8.
Slonim R, C Wang and E Garbarino (2014), “The Market for Blood”, Journal of Economic Perspectives 28(2): 177–96.
Titmuss, R M (1971), The Gift Relationship, London: Allen and Unwin.
Footnotes: 1. Kamakahi v. American Society for Reproductive Medicine, US District Court Northern District of California, Case 3:11-cv-01781-JCS, 2016.
Friday, January 17, 2020
Germany sticks with opt-in donation for deceased donor organs for transplants
German parliament: Explicit consent still necessary from organ donors
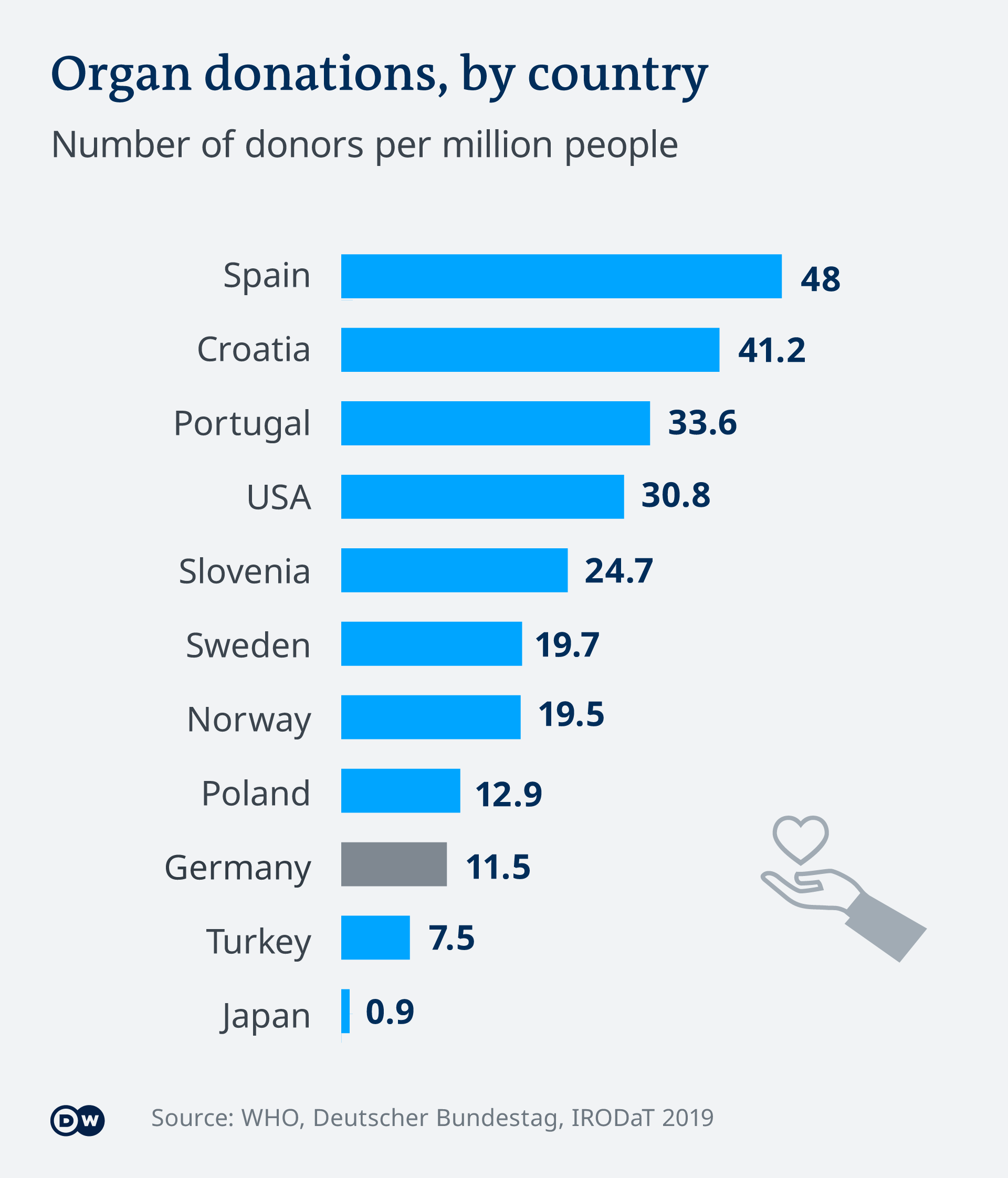
Germany's parliament has rejected a health ministry proposal for a new organ donation system. With low donor numbers, the health minister wanted a presumed-consent system, with the onus on people to refuse to donate.
Date 16.01.2020 Author Mark Hallam, Astrid Prange
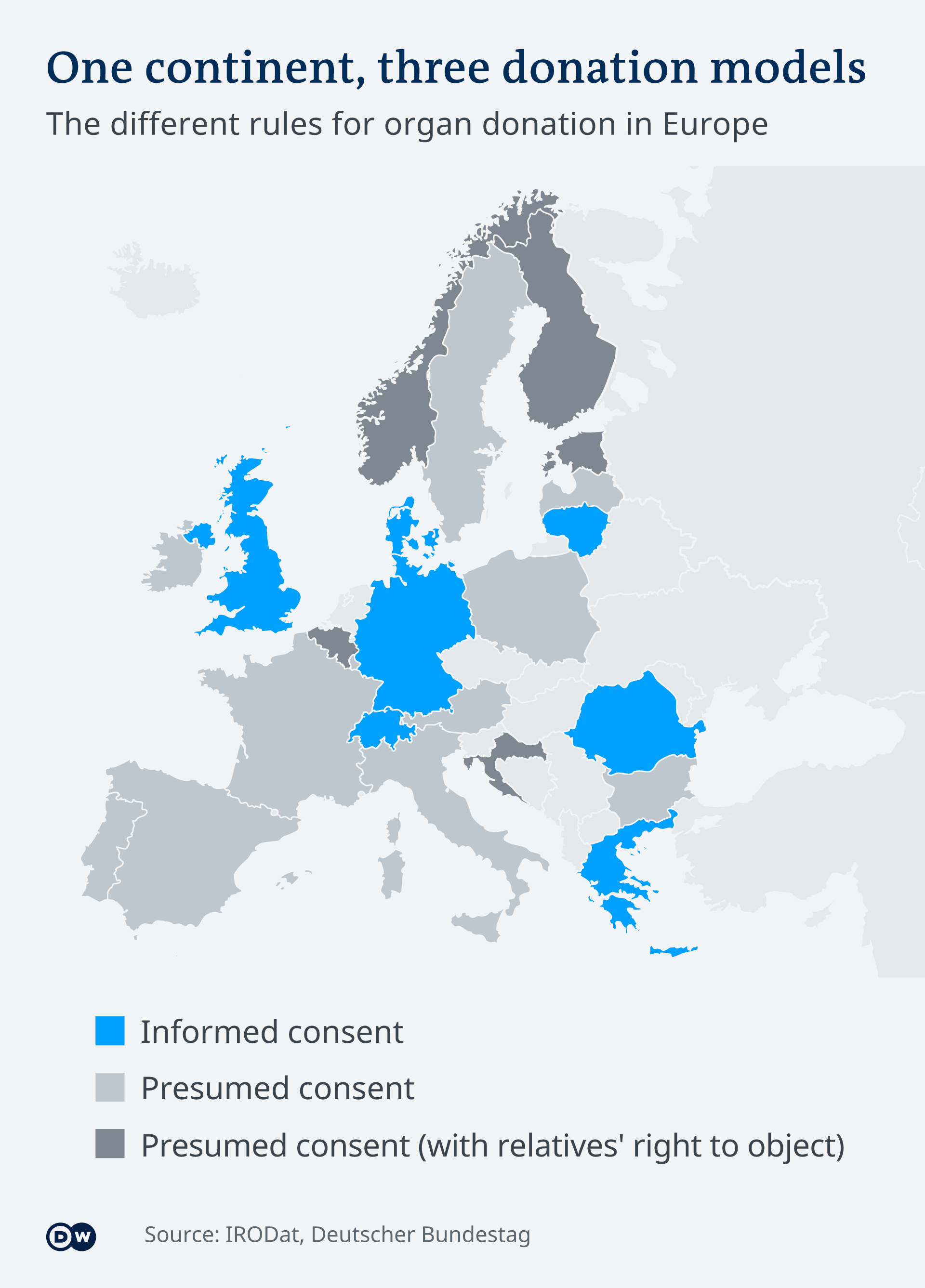
"Germany's organ donation rules will remain largely unchanged after an emotional debate in the Bundestag on Thursday morning. The country will stick with a system of informed consent, whereby only people who voluntarily register as organ donors are eligible. Most, but not all, EU members have moved to an opt-out system that presumes a willingness to donate.
Monday, November 11, 2019
Wednesday, January 30, 2019
Kidney exchange in Germany? It will need an amendment to the Transplantation Act
Google translate renders the opening paragraphs as follows:
"Patients wait a long time for donor organs. That can be changed - with a proposal that has received the Nobel Prize.
Organ donation is literally a matter of life and death. Anyone who receives the urgently needed organ in good time lives on. In Germany, however, many are waiting for the necessary transplantation - often for years. At the same time, the number of organ donations is falling. So how can the number of donated organs be increased so that affected people can live? That's a tricky question, because too many answers tend to limit the voluntary nature of the donation. On Wednesday, the topic is on the agenda of German politics, when the Health Committee of the Bundestag deals with the amendment of the Transplantation Act.
The economists Dorothea Kübler and Axel Ockenfels advise the politicians to take a look at living donations. Kidneys or parts of the liver can also be donated by living people - and this is much less common in Germany than in other countries. The proposal goes in the direction of the FDP parliamentary group around the chairman Christian Lindner, who are pushing for more living donations. In a motion for the health committee on Wednesday, the FDP is proposing to allow the cross-donation of two couples and an anonymous live donation to an organ pool. "
Saturday, September 12, 2015
Ethical issues concerning living donors: a European conference
 |
|
|
Sunday, 13 September, 09:00 - 12:50
|
||
Moderated by: Annette Lennerling, Gothenburg, Sweden and
Willem Weimar, Rotterdam, The Netherlands
|
||
 |
Antonia Cronin: "Is it unethical for doctors to
encourage healthy adults to donate a kidney to a stranger"
Antonia Cronin is Consultant Nephrologist and Honorary Senior Lecturer at the MRC Centre for Transplantation, King's College, London. She is chair of the British Transplantation Society Ethics Committee and appointed member of the UK Donation Ethics Committee. Her presentation will examine the legitimacy of allowing individuals to donate an organ to a stranger and explore the circumstances in which encouraging such a form of donation may be justified. |
|
 |
Willij Zuidema: "Unspecified donors and domino-paired
chains"
Willij Zuidema is working at Erasmus MC in Rotterdam, The Netherlands. For years she is involved in the alternative living donation programs. Especially the program of the unspecified donors has her interest. The living donation program in Rotterdam is one of the largest in Europe with an expertise in unspecified donors and domino-paired chains. She will present the data and logistics of the unspecified donations and domino-paired transplants. |
|
 |
Mihaela Frunza: "Acceptability of public
solicitation, the role of social media"
Mihaela Frunza is Associate Professor at the Department of Philosophy, Babes-Bolyai University, Cluj, Romania. She will present a presentation where public solicitation of organs is critically assessed from a legal, moral, and practical perspective. Several recommendations are discussed that aim at maximizing the organ donor pool while safeguarding the interests of potential living donors. |
|
 |
Leonie Lopp: "The legal debate on anonymous
donation"
Leonie Lopp studied law in Münster, Germany. Afterwards, she wrote her doctoral thesis with the title "Regulations regarding Living Organ Donation in Europe - Possibilities of Harmonisation". She will today present the results of comparing the legal regulations on living organ donation in Europe by focusing on anonymous living organ donation. |
|
 |
Hannah Maple: "Psychological outcomes after
unspecified donation"
Hannah Maple is a trainee Renal Transplant surgeon in London, United Kingdom. She will present an overview of the psychosocial issues pertinent to unspecified donation. Additionally she will discuss the results of her UK based study into psychosocial outcomes after unspecified donation. |
|
 |
Linda Wright: "Ethical and practical issues of
breaking anonymity"
Linda Wright conducts research on transplantation ethics with the Canadian National Transplant Research Programme in Toronto, Canada. She will discuss the experience of contact between anonymous living donors and their recipients and recommend a strategy to address this, in the absence of evidence to support best practice. |
|