Here are two recent reports of the first cross-border transplant between China proper and Hong Kong.
From the Global Times:
First organ donation between mainland and HK saves 4-month old baby By Wan Hengyi
"A medical team of the Hong Kong Children's Hospital successfully transplanted a heart donated from the mainland to a 4-month-old baby in Hong Kong Special Administrative Region on Saturday, achieving a historic breakthrough in the sharing of human organs for emergency medical assistance between the two places for the first time.
"The donated heart, which had been matched by China's Organ Transplant Response System (COTRS) through several rounds and had no suitable recipient, was successfully matched in Hong Kong through the joint efforts between 24 departments and 65 medical experts in the mainland and Hong Kong.
"Cleo Lai Tsz-hei, the recipient of the transplant from Hong Kong, was diagnosed with heart failure 41 days after birth and was in critical condition. Receiving a heart transplant was the only way to keep her alive, according to media reports.
"Moreover, the acceptable heart donation for Cleo requires a donor weighing between 4.5 kilograms and 13 kilograms, and the chances of a suitable donor appearing in Hong Kong are slim to none.
...
"COTRS initiated the allocation of a donated heart of a child with brain death due to brain trauma in the mainland on December 15. As a very low-weight donor, no suitable recipients were found after multiple rounds of automatic matching with 1,153 patients on a national waiting list for heart transplants in the COTRS system. In the end, the medical assistance human organ-sharing plan between the Chinese mainland and Hong Kong was launched.
"Some netizens from the Chinese mainland asked why a baby from Hong Kong who has not lined up in the COTRS system can get a donated heart when there is a huge shortage of donated organs in the mainland.
"In response, the organ coordinator told the Global Times that the requirements for organ donation are extremely high, noting that all the prerequisites including the conditions of the donor and recipient, the time for the organ to be transported on the road and the preparation for surgery must reach the standards before the donation can be completed.
"The COTRS system has already gone through several rounds of matching, which is done automatically by computer without human intervention, said the organ coordinator.
"Medical teams from both jurisdictions, as well as customs officers in Shenzhen and Hong Kong, carried out emergency drills to reduce the customs clearance time to eight minutes, racing against the four-hour limit for preserving donated hearts, said Wang Haibo, head of the COTRS for medical assistance contact between the mainland and Hong Kong.
"The collection of donated hearts began at 17:00 pm on Friday, and the hearts were delivered to the Hong Kong Children's Hospital at 20:00 pm under the escort of Hong Kong police on the same day. At 1:00 am on Saturday, Cleo's heart transplant operation in Hong Kong was successfully completed, and she has not required extracorporeal circulation support at present."
********
And from the South China Morning Post:
Hong Kong could greatly benefit from cross-border organ imports mechanism, doctors say after local baby receives heart from mainland China by Jess Ma
"Hong Kong could greatly benefit from cross-border organ donations given the city’s persistently low rate of residents willing to sign up to become donors, doctors have said after a local baby girl received a heart from mainland China in the first arrangement of its kind.
...
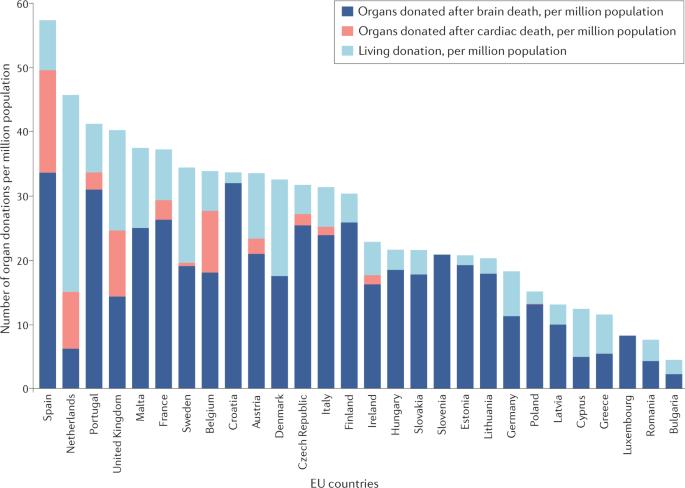
"Hong Kong’s organ donation rate is currently among the lowest in the world, at 3.9 donors per a million people in 2019, down from 5.8 in 2015, according to research conducted by the Legislative Council.
...
"Medical lawmaker David Lam Tzit-yuen and election committee legislators Elizabeth Quat Pei-fan and Rebecca Chan Hoi-yan urged the government to begin discussions on legal frameworks and procedures for cross-border transplants, saying that the mainland had a robust donation system and that organ sharing between the city and the mainland was not unusual.
"Human rights groups and lawyers have accused the mainland of forcibly harvesting organs from executed prisoners, a practice that then health minister Huang Jiefu publicly acknowledged in 2005. The government announced in 2015 that organ donations would only come from “voluntary civilian organ donors,” but critics argued prisoners were not excluded under the system.
But Chan argued that the mainland’s efforts to improve the transparency and ethics of its organ donation system over the past decade should be acknowledged.
“I disagree that this would be the beginning of a slippery slope. The transparency of the mainland’s organ donation system has been a lot clearer and stricter,” Chan said, adding that a lot of work had been done across the border to prohibit organ harvesting and trading."