Elaine Perlman forwards the following discussion points:
Coalition
to Modify NOTA Talking Points
modifyNOTA.org
What is the Coalition to Modify
NOTA proposing? The Coalition to Modify NOTA proposes providing a $50,000
refundable tax credit to remove all disincentives for American non-directed
kidney donors who donate their kidney to a stranger at the top of the kidney
waitlist in order to greatly increase the supply of living kidney transplants,
the gold standard for patients with kidney failure.
What is the value of a new kidney? The value
of a new kidney, in terms of quality of life and future earnings potential, is
between $1.1 million
and $1.5 million.
What is the American kidney
crisis? Fourteen Americans
on the waiting list for a kidney transplant die each day. That number does not
include the many kidney failure patients who are not placed on the waiting list
but would have benefited from a kidney transplant if we had no shortage. The total
number of Americans with kidney failure will likely exceed one million by 2030.
Why not
rely on deceased donor kidneys to end the shortage? A living
kidney transplant lasts on average twice as long as a deceased donor kidney.
Fewer than 1 in 100 Americans die in a way that their kidneys can be procured.
Currently, the 60% of
Americans who are registered as deceased donors provide kidneys for 18,000
Americans annually. Even if 100% of Americans agreed to become organ donors,
this would raise donations by only about 12,000 per year. In the
USA, 93,000
Americans are on the kidney waitlist. A total of 25,000 people
are transplanted annually, two-thirds from deceased donors and one-third from
living donors. The size of the waitlist has nearly doubled in the
past 20 years, while the number of living donors has not increased.
What is the
extra value that non-directed kidney donors provide? Non-directed
kidney donors often launch kidney chains that can result in a multitude of Americans receiving
kidneys. Fewer than 5% of all living kidney donations are from
non-directed kidney donors who are an excellent source of organs for
transplantation because they are healthier than the general population.
How much
does the taxpayer currently spend on dialysis? Kidney
transplantation not only saves lives; it also saves money for the taxpayer. The
United States government spends nearly $50 billion
dollars per year (1% of all $5 trillion collected in annual taxes) to pay
for 550,000 Americans
to have dialysis, a cost of approximately $100,000 per year per patient, a
treatment that is far more expensive than transplantation.
How many
more lives will be saved with the refundable tax credit for non-directed
donors? The number of non-directed donors increased from 18 in 2000 to
around 300 each year. After our Act becomes law, we estimate that we will add
approximately 7,000 non-directed donor kidneys annually. That is around 70,000
new transplanted Americans by year ten.
How much
tax money will be saved once the Act is passed? The
refundable tax credit will greatly increase the number of living donors who
generously donate their kidneys to strangers. We estimate that in year ten
after the Act is passed, the taxpayers will have saved $12 billion.
What is a
refundable tax credit? A refundable tax credit can be accessed by both
those who do and those who do not pay federal taxes.
What do
Americans think about compensating living kidney donors? Most
Americans favor compensation for living kidney donors to increase
donation rates.
Who is able to donate their
kidneys? Donation requires potential organ donors to undergo a
comprehensive physical and psychological evaluation, and each transplant center
has its own rigorous criteria. Only around 5% of those who pursue evaluation
actually end up donating, and only about one-third of Americans are healthy
enough to be donors. Providing financial incentives will encourage more
Americans to donate their kidneys to help those with kidney failure.
Do kidney donors currently have
expenses that result from their donation? The medical costs of
donation are covered by the recipients' insurance, but donors are responsible
for providing for the costs of their own travel, out-of-pocket expenses, and
lost wages. Programs like the federal NLDAC and NKR's Donor Shield can help
offset these costs, making donation less expensive.
Is it moral to compensate kidney
donors? Compensation for kidney donors can be viewed as a way to
address the current kidney shortage and save lives. Americans are compensated
for various forms of donation such as sperm, eggs, plasma, and surrogacy, all
of which involve giving life.
How long do we need to compensate
living kidney donors? Compensation should continue until a xenotransplant or advanced
kidney replacement technology becomes available. In the meantime, it's crucial
to prevent further loss of lives due to the shortage.
Will incentivizing donors
undermine altruism? Financial compensation for donors can coexist
with altruism. Donors can opt out of the funds from the tax credit or choose to
donate those funds to charity. The majority of donors support financial
compensation, and relying solely on altruism has led to preventable deaths.
In addition to ending the kidney
shortage, what are other benefits of the Act? The Act can help combat
the black market for kidneys and reduce human trafficking because we will have
an increased number of transplantable kidneys. It can also motivate individuals
to become healthier to pass donor screening, potentially further reducing
overall healthcare costs.
Why provide non-directed donors
with a refundable tax credit of $50,000? The compensation is designed to
attract those who are both healthy and willing to donate. Given the commitment,
time, and effort involved in the donation process, this compensation recognizes
the value of those who save lives and taxpayer funds.
When more donors step forward,
can transplant centers increase the number of surgeries? There is
considerable unused capacity at most U.S. transplant centers, and increasing
the number of donors is likely to lead to more surgeries. The goal is to
perform more kidney transplants and reduce the waitlist, benefiting patients in
need.
In what way does the Act uphold The Declaration of Istanbul? While
the Act deviates from one principle of the Declaration of Istanbul by offering
compensation, it aligns with the other principles and is expected to
standardize compensation and reduce worldwide organ trafficking.
What about dialysis as an
alternative to transplant? Dialysis, while a treatment option,
can be a challenging and uncomfortable process for patients. For those who
could have been transplanted if there were no kidney shortage, dialysis can
result in needless suffering and an untimely death.
Why not compensate living liver
donors? Liver donation is riskier and not as cost-effective as kidney
donation. While the Act currently focuses on kidney donors, it's possible that
compensation for liver donors could be considered in the future.
What about the argument that
providing an incentive to donate will exploit the donors, especially low income
donors?
Primarily middle and low income
kidney failure patients are dying due to the kidney shortage. People with lower
incomes tend to have social networks with fewer healthy people because health
is related to income level. In addition, being placed on a waitlist often costs
money. Kidney donation also costs money, an estimated 10% of annual
income. The refundable tax credit will help low income donors and recipients
the most by making donation affordable and increasing the number of kidneys for
those waiting the longest on the waitlist, frequently middle and low income
Americans. The tax credit aims to help those most affected by the kidney
shortage, as poorer and middle-income individuals often bear the brunt of the
kidney crisis’s consequences. The Act will level the playing field, making it
easier for those at all income levels to receive a life-saving kidney.
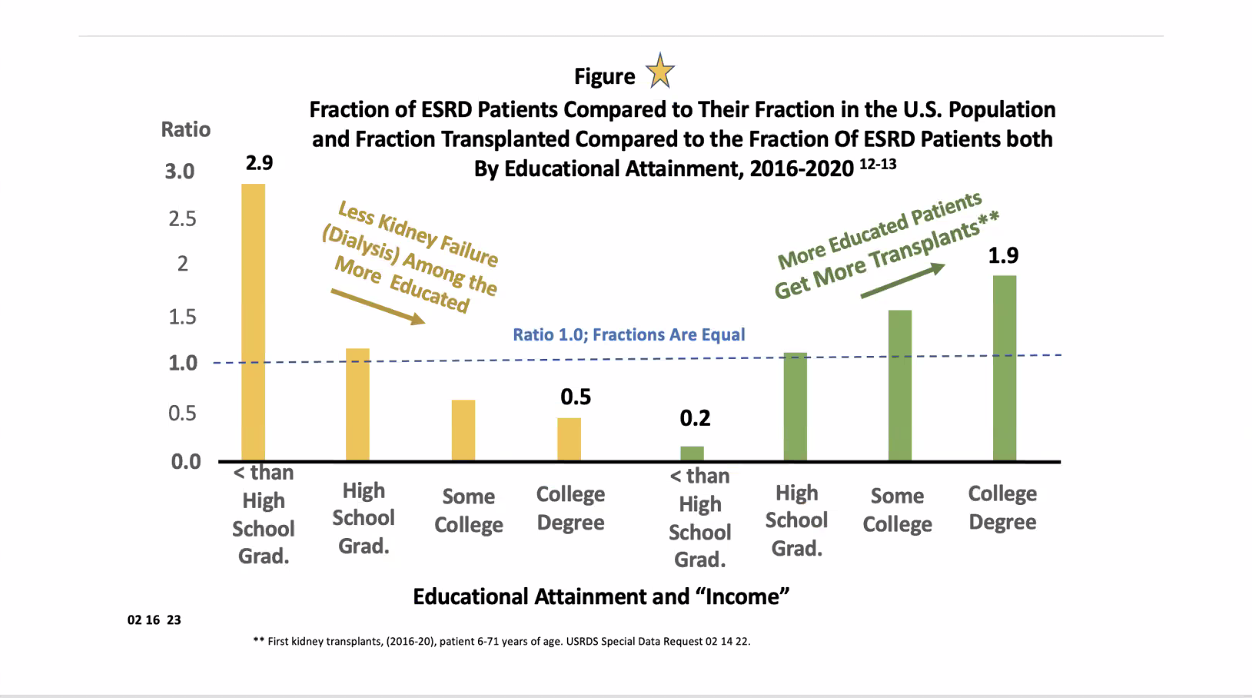
Please examine this chart: